Have an opinion about this issue of PAW? Please take a minute to click here and fill out our online questionnaire. It’s an easy way to let the editors know what you like and dislike, and how you think PAW might do better. (All responses will be anonymous.) |
May 11, 2005: Features
 Desperate
Remedies
Desperate
Remedies
Embrace of a deadly cure
By Andrew Scull *74
On Jan. 11, 1921, at 4:30 in the afternoon, Henry Aloysius Cotton, the superintendent of the New Jersey State Hospital in Trenton, rose to address a packed house at Princeton. The audience, numbering nearly 400, had assembled in McCosh 10 to hear him deliver the first of four Vanuxem lectures. Louis Clark Vanuxem 1879’s bequest in 1912 had endowed a series of annual public lectures at his alma mater, and he had specified that at least half of them were to be on subjects of current scientific interest. Over the course of the 20th century, his generosity would bring a galaxy of distinguished scholars to the university — luminaries like Edwin Hubble, Thomas Hunt Morgan, Robert Oppenheimer, John Von Neumann, Linus Pauling, Harold Urey, and Francis Crick. And then there was Cotton, the lone representative of the marginal and often stigmatized field of psychiatry. What explains his presence in the pantheon?
(Photographs courtesy New Jersey State Archives, Department of State; Photo montage by Steven Veach)
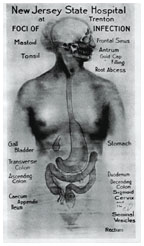
Cotton used a version of this diagram on multiple occasions to illustrate the often obscure nooks and crannies of the body where focal sepsis could lurk undetected, spreading its poisons into the system and prompting a descent into madness. (photographs courtesy New Jersey State Archives, Department of State)
Henry Cotton at work in his office at Trenton State Hospital around the late 1920s.
Doctors working as consultants to Cotton perform abdominal surgery on a patient with mental illness at Trenton State Hospital. Cotton would later perform these operations himself. (New Jersey State Archives, Department of State) |
Certainly, Henry Cotton had a glittering résumé, at least by the standards of his field. Early training at the University of Maryland and at Johns Hopkins had been followed by an appointment to an extremely competitive post under the figure who would dominate American psychiatry in the first half of the 20th century, the Swiss-born and -trained Adolf Meyer. Further research in Germany under psychiatrists Emil Kraepelin and Alois Alzheimer gave Cotton a scientific pedigree that few “alienists” — the term then used to describe physicians specializing in the treatment of mental disorders — of his age could match. Cotton’s selection to head New Jersey’s premier asylum, at the age of barely 30, marked him as one of the most promising psychiatrists of his era. On that January day at Princeton, he rose to announce a breakthrough in the understanding and treatment of mental disorder, a breakthrough that in his eyes, and the eyes of his sponsors (who included leading scholars in Princeton’s biology department), was every bit as important as the advances in astronomy, embryology, game theory, nuclear physics, molecular biology, and chemistry that other Vanuxem lecturers would discourse on.
Not for Cotton the orthodox position embraced by most psychiatrists of his age: the belief that major mental disorders were rooted in faulty heredity, in biological defects that marked those suffering from them as degenerate representatives of the human race. But neither did he accept the recently fashionable notion propounded by Freud and his followers: that mental illness was rooted in childhood traumas, in the collision of unconscious forces, in the pathologies of the psyche. There, in Cotton’s view, lay the road to quackery and pseudo-science. Instead, he announced his startling new theory of the origins of mental illness, one that reduced the myriad manifestations of madness to a single underlying cause. Simultaneously, he said, he had uncovered a straightforward therapeutic that grew directly out of his etiological discoveries, one that promised to cure upwards of 85 percent of cases of psychosis – and even, if employed prospectively, to eliminate mental disorders altogether.
The key, Cotton argued, was germs. Germs and pus. For years, conservative medical men had resisted the implications of the work of such scientists as Louis Pasteur and Robert Koch, and the warnings about the perils of pus in the practice of surgery that emanated from the apostle of antiseptic surgery, Joseph Lister. But by the dawn of the 20th century, the gospel of “germs” was sweeping all before it. Medicine embraced the laboratory as a source of cultural authority. Bacteriological models of disease brought gains in etiological understanding and, to a more limited degree, in therapeutic efficacy. The upshot was that physicians and surgeons, donning the mantle of the new science, found their prestige and their prospects soaring. And yet there were diseases and disorders that remained recalcitrant, resistant to the new paradigm, and frustratingly beyond the reach of modern therapeutics: rheumatism and arthritis, for example, and atherosclerosis and nephritis.
In the second decade of the 20th century, a number of physicians began to embrace the notion that these conditions, too, were a manifestation of the malevolent impact of germs. The men who advanced this hypothesis were anything but marginal figures: They included the dean of the medical school at the University of Chicago and prominent clinicians at such major centers of modern scientific medicine as the Mayo Clinic in Minnesota and the Johns Hopkins medical school in Baltimore. Their conviction grew that a whole array of hitherto mysterious and untreatable illnesses in fact derived from something they called focal sepsis. Chronic, low-grade infections lurking unnoticed in obscure regions of the body pumped out poisons — powerful toxins that, as they spread through the bloodstream and the lymph, produced pathological action at a distance, and were thus responsible for a whole array of baffling diseases.
Cotton seems to have encountered these notions sometime around 1915. He was scarcely the only alienist to wonder whether they might have applications in psychiatry, but he was certainly the most aggressive and single-minded in pursuing their implications. He at once set to work to bring blood tests, X-ray machines, microscopes, and test tubes to Trenton, along with an array of outside consultants to help locate and eliminate the sources of sepsis. Over the next five years or so, his conviction that he had uncovered the single source of psychosis hardened into certainty, and he developed a whole range of therapies designed to combat the perils of pus infection. At Princeton, he laid his theories and his therapeutic breakthroughs before the educated and influential audience that had gathered to hear him speak.
Depression, delusions, hallucinations, mania, indeed all manner of mental disturbances were, he informed his listeners, but the surface manifestations of an underlying physical disorder of a quite familiar infectious source. More remarkably still, once the source of the infection was tracked down and eliminated, the return of mental stability was assured. And in an era that possessed no penicillin or other antibiotics, the process of elimination required a resort to “surgical bacteriology” — put more plainly, cutting out the roots of the trouble.
As early as 1916, Cotton had begun to attack and remove the most obvious site of infection, the teeth: unerupted and impacted teeth; teeth with infected roots and abscesses, decayed or carious teeth, apparently healthy teeth with periodontitis, poorly filled teeth, sclerotic teeth, teeth with crowns. When many of his patients stubbornly refused to recover, he was undeterred, redoubling his efforts to locate the underlying focal sepsis he felt certain was there. Tonsils and sinuses were soon joined by spleens and stomachs, colons and cervixes, as he ruthlessly pursued his goal of a thorough cleansing of his patients’ bodies. And the results, he informed his rapt Princeton audience, were little short of astonishing. In his final lecture, he reviewed case after case of patients seemingly condemned to a lifetime of mental darkness who, once relieved of their infected teeth, tonsils, stomachs, or colons, made near-miraculous recoveries.
At the State Hospital, not far from the Princeton campus, a full-fledged surgical assault on sepsis was now the order of the day. Each year, thousands of teeth and tonsils were extracted, and scores of colons and other internal organs sectioned and removed. The payoff, Cotton proclaimed, was a massive increase in the number of cures, and an equally major savings to the state’s treasury.
When the New York Times reviewed the published version of Cotton’s Princeton lectures in June 1922, its reviewer, Thomas Quinn Beesley, had no doubt of their importance: “At the State Hospital at Trenton, N.J., under the brilliant leadership of the medical director, Dr. Henry A. Cotton, there is on foot the most searching, aggressive, and profound scientific investigation that has yet been made of the whole field of mental and nervous disorders.” Across the country, others had given way to despair, as rates of mental illness grew four times as fast at the general population, the Times noted. But thanks to Cotton, it said, “there is hope, high hope ... for the future.”
Desperate for relief from the demons that tormented them (or their nearest and dearest), and dazzled by the seemingly authoritative reports emanating from Trenton about the extraordinary breakthroughs associated with a bacteriological model of madness, patients and their families urgently sought to share in the new miracle cures. Affluent madmen and madwomen flocked to Trenton, their numbers originally swelling the ranks of those confined at the State Hospital, where their willingness to pay premium rates for the attention of Cotton and his consultants made them a highly desirable commodity. Across the country, alienists reported that they found themselves besieged by supplicants seeking the new wonder cure. Frantic families urged that teeth, tonsils, and guts be ransacked for the source of the germs that prompted hallucinations and delusions, ranting and raving, dolor and depression. For so long, madness had seemed a condition beyond help, a source of stigma and shame. If modern biological science had revealed that it was just another physical affliction, no more than the effects of bacterial poisoning of the brain, then deliverance might be at hand.
The case of Margaret Fisher, one of the first private patients to be transferred to Trenton, illustrates the eagerness with which highly educated and well-connected people arrived to be treated with Cotton’s miraculous new therapies, and brought their relations to receive treatment at his hands. Margaret was the daughter of Irving Fisher, a Yale professor lionized by no less a figure than Joseph Schumpeter as “the greatest economist that America has produced.” Irving Fisher was an arrogant, humorless, and domineering man who made and eventually lost a fortune exceeding $10 million (well more than $40 million in today’s dollars), enjoyed access to the highest circles of American society, and embraced a host of causes, including Prohibition, eugenics, dietary reform, and the extension of the human life span.
Developing close ties with John Harvey Kellogg, patriarch of the immensely fashionable Battle Creek Sanitarium in Michigan (and founder of the breakfast cereal empire), Fisher had begun in the early 1900s to take his wife and family there each year to partake of the cure. Hydrotherapy, exercise, a vegetarian diet, close attention to the working of the bowels — all these central elements of Kellogg’s regime became a regular part of the Fisher family routine. As a dutiful daughter, Margaret embraced such “healthy” practices at her father’s urging.
Still living at home as she entered her 20s, and serving as an unpaid office assistant to her father, Margaret seems to have undergone a slow mental deterioration beginning about 1916. The changes were subtle at first, the onset of her symptoms insidious and easy to overlook or rationalize. Only in retrospect did her parents come to see them as signs of incipient pathology.
On April 27, 1918, Margaret became engaged to be married. Her parents were delighted, and Margaret’s father, having checked the young man’s pedigree with one of his oldest friends, urged her to marry as soon as possible. But the prospect seems to have unhinged her. Within days, as Cotton later noted in the last of his Vanuxem lectures (though without mentioning Margaret by name), she began to babble “queer things about portents and was afraid her fiancé would not come back [from the war]. She soon began to talk at random about ‘God, Christ, and immortality,’ and reacted to auditory hallucinations. Her conduct was peculiar in many ways. Her condition gradually became worse, and on June 1 she had to be sent to a private hospital.”
Thus far, the Fishers had defined her condition as a temporary nervous prostration, and kept her out of any sort of psychiatric facility. Unfortunately, however, once hospitalized, as Cotton’s case notes recorded, “she became much worse, and could not be controlled” – so their hands were forced. Fisher and his wife concluded “it was necessary to send her to the Bloomingdale Asylum” in White Plains, long regarded by America’s plutocrats as a suitable institution for those of their social class. Admitted on June 27, Margaret was “pensive and preoccupied, and at times depressed. She responded slowly to questions and when aroused was irrelevant.”
Her psychiatrists soon despaired of her prospects. Noting the “acute distortion of the patient’s personality with marked distortion in thinking, peculiar behavior, and disharmony between mood and thought content,” they concluded, as Cotton faithfully noted, that her psychosis “seems more nearly related to the schizophrenic disorders than to the exhaustive or manic-depressive disorders.” These were important diagnostic distinctions, since schizophrenia in this era was widely felt to be an essentially incurable condition. Indeed, the Fishers were informed that “a recovery without defect symptoms seems improbable.” Irving Fisher’s response was swift: He arranged to have Margaret released from Bloomingdale on March 29, 1919, and that same day she was spirited out of the state and admitted as a private patient to Trenton State Hospital.
Over the years, Fisher had maintained close contacts with John Harvey Kellogg. In August 1914, for instance, the two men had jointly organized the First International Congress on Racial Betterment in Battle Creek, and Fisher had written for Kellogg’s magazine, Good Health. Kellogg, like Cotton, emphasized the nefarious influence of decayed teeth and the poisons that lurked in the bowels, so when Fisher learned of Cotton’s assertions about the etiological connections between focal sepsis and insanity, and the possibility of intervening to cure the apparently hopeless through a program of surgical bacteriology, he was already primed to accept these claims.
Neurologically, Cotton reported, Margaret Fisher seemed normal. But there was ominous evidence of “marked retention of fecal matter in the colon with marked enlargement of the colon in this area.” To be sure, “Because of her resistiveness, X-ray studies of the intestinal tract could not be made,” but Cotton was convinced that the source of a substantial portion of her problems had been uncovered. Proceeding further, he found evidence that her “cervix was eroded.” Deeply suspect as well were two unerupted molars, which Cotton immediately insisted must be extracted. He next approached the Fishers for permission to perform “an exploratory laparotomy [a surgical opening of the abdomen to examine the internal organs] based upon the physical examination and the fact of long-continued constipation.”
Irving Fisher and his wife obviously were eager to embrace this somatic account of their daughter’s disorder. It provided an etiological account in close accord with their own beliefs about human health, and a far more hopeful prognosis than the one the doctors at the Bloomingdale Asylum had delivered. Still they hesitated to endorse so drastic a remedy as surgery on Margaret’s bowels, announcing that they “preferred to wait till other means such as vaccine and serum should be exhausted.” In August, however, they did consent to removal of a portion of Margaret’s cervix after being advised of the presence of “pure colon bacillus” in her tissues. The operation was performed by Cotton’s assistant, Dr. Robert Stone, on Aug. 15, 1919, and the following day, Fisher and Cotton took the train to Battle Creek to consult with Kellogg about how to proceed. Seizing the opportunity presented by their extended time together, Cotton was clearly doing all he could to overcome Fisher’s hesitations about further surgery for his daughter. Fisher wrote to his wife, “Dr. C. doesn’t think M will suffer any pain. The uterus, like the intestines and other internal organs, has few nerves.” Fisher reminded his wife that Cotton believed the bowels were another source of infection that needed attention.
Yet still Margaret’s parents hesitated. Back at the hospital, Cotton acknowledged that “the family preferred to wait. ... So in September another course of antistreptococcous [sic] treatment was given.” Again he urged surgery on the bowels. Again Fisher temporized: “As to operating on M,” he wrote to his wife in early October, “we’ll talk it over with Dr. C. and each other.” And then events took the decision out of their hands.
Perhaps the crisis was iatrogenic, the result of a failure to kill the streptococci before injecting them into poor Margaret’s body. In any event, in late October Margaret exhibited symptoms of inflammation of the lungs, and a deep-seated abscess developed over the ribs on her left side — an abscess that, when lanced and cultured, Cotton recorded, “gave pure streptococcus ... the same type found in the teeth and stomach. The condition of the patient did not improve and her temperature continued to be high. She failed rapidly and died on Nov. 7, 1919.”
Despite Margaret’s death, Cotton believed her case demonstrated the septic origins of psychosis. Fisher, though devastated by the outcome, continued to believe in Cotton’s theories, and to insist that there had been a physical cause of his daughter’s illness. “Even years later,” according to one of Fisher’s biographers, Robert Loring Allen, “he wrote his friend Will Eliot that some form of toxemia causes a nervous breakdown.” Of course, such sustained faith was a natural psychological defense mechanism in the face of the choices he had made and the treatments he had authorized, but it also reflected how stubbornly Fisher held to his beliefs, not just on this front, but on a whole range of issues. And Fisher was clearly not alone. Legions of other well-to-do Americans followed in his footsteps, so many that the number of private patients showing up in Trenton to receive treatment began to exceed the capacity of the State Hospital to receive them. As their ranks swelled, Henry Cotton seized the opportunity to open a private hospital in Trenton, an establishment to which the bulk of these paying patients were henceforth referred for treatment.
The claimed cures, of course, were spurious. Yet Cotton continued to
pursue focal sepsis with fierce determination for more than a dozen years
after his Princeton lectures. None of his professional brethren made more
than the feeblest effort to rein him in, even though in further publications,
he acknowledged that his abdominal surgery was attended with a mortality
rate of some 30 percent. (The actual rate, subsequent close study of the
hospital records would indicate, was nearly 45 percent.) When Cotton’s
patron, Adolf Meyer, was presented with a meticulous report from a brave
female associate whom he had sent to evaluate the work — a report
that showed the approach adopted at Trenton to be useless and massively
harmful — he suppressed its findings and allowed the slaughter to
proceed. By the time Cotton dropped dead of a heart attack at his private
club in Trenton, in May 1933, hundreds of patients had died and thousands
more had been maimed. Although abdominal surgery ceased with his death,
Cotton’s other techniques continued to be used for almost three
decades as a succession of his protégés were named superintendent
at Trenton. His victims, sadly, included even his own sons, Henry Jr.
’30 and Adolph ’31, stripped of their teeth as a prophylactic
measure prior to their matriculation at Princeton. Both later killed themselves.
![]()
Andrew Scull *74 is Distinguished Professor of Sociology and Science Studies at the University of California, San Diego. His book about Henry Cotton, Madhouse, will be published by Yale University Press this month.