A team of scientists employing a sophisticated computer model pioneered at Princeton University and Resources for the Future has found that many governments worldwide are recommending the wrong kind of malaria treatment.
Despite the availability of many drugs and therapies to treat malaria, many countries' national policies recommend using what is known as a single first-line therapy -- that is, using one drug repeatedly with many patients. Writing in the Sept. 16 issue of the Proceedings of the National Academy of Sciences, a team led by Maciej Boni, who conducted the research as a postdoctoral fellow at Princeton and scholar at Resources, a Washington, D.C.-based think tank, reports that countries could cut the death rate and forestall the development of drug resistance if a variety of different drugs were distributed to patients.
This approach, known as multiple first-line therapies or MFT, could be put into place by making sure different drugs cost about the same, so that patients would not be forced into buying the cheapest available drug but would choose from a random pool. Or it could be applied by clinic physicians who could simply alternate their choices for drugs they prescribe to patients.
"What we found is that using multiple first-line therapies is the best way to avoid treatment failures and to delay the development of resistance for as long as possible," said Boni, who recently has joined the staff of the Oxford University Clinical Research Unit in Ho Chi Minh City, Vietnam.
One catch to the researchers' strategy is that multiple effective therapies may not always be available. In some African countries where drug-resistance is already widespread, the only effective therapies are a class of drugs known as artemisinin-based combination therapies (ACTs).
"MFT does not necessarily solve all our problems," said Boni. "Antimalarial drug development needs to continue with the hope of producing novel and highly effective antimalarials that can be deployed alongside ACTs."
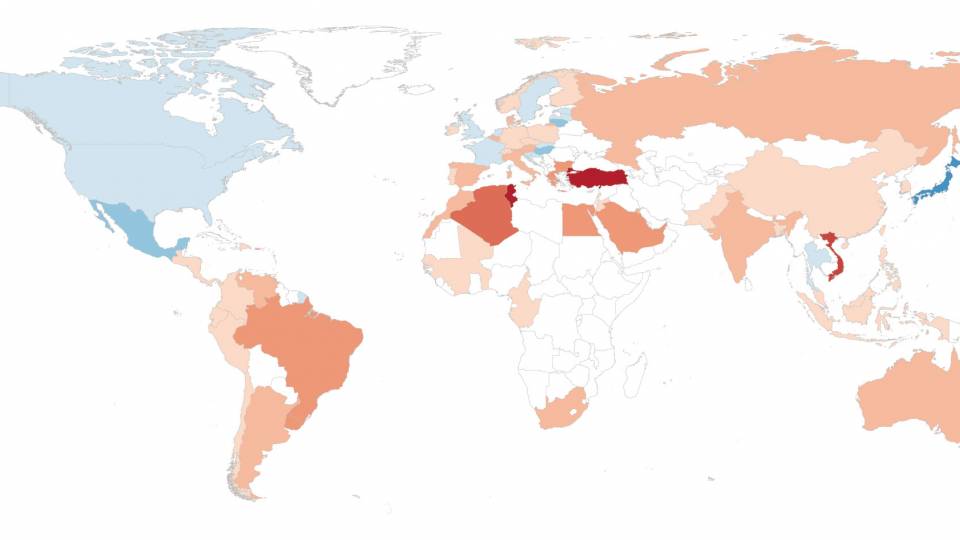
Some 350 to 500 million people are infected with malaria every year by being bitten by a mosquito carrying one of the four human malaria parasites, P. falciparum, P. vivax, P. malariae or P. ovale, according to statistics maintained by the World Health Organization. Falciparum infections are by far the most common, killing more than 1 million people each year. Malaria also contributes indirectly to many more deaths, mainly in young children, among those already suffering from other infections and illnesses. About 60 percent of the cases of malaria worldwide and more than 80 percent of malaria deaths occur in sub-Saharan Africa.
Boni, a mathematician as well as an evolutionary biologist, and his co-authors, Ramanan Laxminarayan and David Smith, designed a computer model with inputs based on more than 100 years of malaria field research. They simulated dozens of treatment paths for a malaria outbreak among patients contrasting many variations of the status quo strategy of using a single first-line therapy with one employing MFT.
They found there were major benefits to employing an MFT strategy, namely, fewer cases of malaria, fewer unsuccessful drug treatments, and a very significant delay in the onset of drug resistance in the parasites. As parasite resistance to antimalarial drugs is the key factor that can make drugs obsolete and useless, delaying and slowing down the evolution of drug-resistance is often viewed as a public health priority when designing strategies for eliminating or controlling malaria.
The computerized analysis conducted by the team represents the most extensive look yet at the question of what works best for large-scale and long-term malaria control. Boni, whose research focuses on the public health consequences of the evolution of infectious diseases, said their study was largely influenced by the work of the theoretical ecologist Simon Levin. Levin, the George M. Moffett Professor of Biology at Princeton, has over the past four decades pioneered techniques that apply rigorous mathematical analysis to biological problems, paving the way for work such as this, according to Boni.
Boni, who earned his bachelor's degree in mathematics from Princeton in 1999, has been a postdoctoral fellow in Levin's lab as well as in the Princeton Environmental Institute. Laxminarayan is both an economist at Resources for the Future in Washington, D.C., and a visiting research scholar at the Princeton Environmental Institute. Smith, who earned his doctoral degree in ecology and evolutionary biology from Princeton in 1998, is a mathematical epidemiologist and faculty member at the University of Florida.
The work was funded by the Bill and Melinda Gates Foundation and the National Institutes of Health.